Linking Sleep Quality with Tau Pathology
The FNSS mutation and tau accumulation
Sleep is essential for maintaining overall health, and chronic sleep deprivation significantly increases the risk of Alzheimer’s disease and other forms of neurodegeneration. Interestingly, individuals with the familial natural short sleep (FNSS) trait experience lifelong short sleep durations without adverse health effects or age-related diseases. The ADRB1 mutation, which causes an alanine-to-valine substitution in the fourth transmembrane region of the β1-adrenergic receptor, is linked to FNSS. This mutation enhances wakefulness and reduces the need for sleep. To study the effects of this mutation, researchers used heterozygous Adrb1-A187V mice, which carry one mutant allele and one normal allele as a model for human mutation carriers.
To investigate the impact of the FNSS-linked mutation on tau pathology, a team of investigators at the University of California, San Francisco crossed heterozygous Adrb1-A187V mice with transgenic PS19 tau mice. The PS19 model expresses the full-length human tau (1N4R) isoform with the P301S mutation, which drives the development of mature tau pathology and neurodegenerative symptoms. Remarkably, the Adrb1-A187V mutation demonstrated a protective effect against tau pathology, reducing the accumulation of hyperphosphorylated tau protein in the piriform cortex (PC) and entorhinal cortex (EC)—two brain regions critical for cognition and memory.
Phosphorylated tau in the blood is a promising biomarker for Alzheimer’s disease, as it closely reflects tau pathology in the brain. In the Adrb1-A187V PS19 mice, the ratio of phosphorylated tau to total tau protein was significantly lower than in the PS19 tau model alone, further confirming the protective role of the Adrb1 mutation. These findings highlight the potential of targeting sleep-related pathways to mitigate tau-related neurodegeneration.
Implications for sleep quality
In the next phase of the study, researchers examined pathologically phosphorylated tau in the locus coeruleus, a brain region that releases norepinephrine, the ligand for the β1-adrenergic receptor. Known as the sleep-wake center, the locus coeruleus is one of the first areas to exhibit Alzheimer’s disease-like neuropathology, including increased levels of phosphorylated tau and neuronal loss.
Chronic sleep deprivation in the PS19 tau mouse model was found to exacerbate tau pathology and lead to a significant reduction in locus coeruleus neurons, even in young adult mice. Analysis of this brain region revealed that mice carrying the Adrb1-A187V mutation had reduced levels of phosphorylated tau, supporting the findings from earlier parts of the study. Notably, total tau levels remained similar across both genotypes.
The investigation then turned to how the Adrb1-A187V mutation influenced physiological processes such as sleep quality. Previous studies have shown that Alzheimer’s disease is associated with disruptions in rapid eye movement (REM) sleep, which is linked to cognitive decline. Using continuous electroencephalography (EEG) and electromyography (EMG) monitoring, sleep physiology was assessed under normal conditions and following sleep deprivation. While no significant changes were observed in total sleep duration or non-REM sleep, REM sleep was notably impacted. The PS19 tau mouse model demonstrated a loss of REM sleep, a critical phase of sleep associated with vivid dreaming and memory consolidation. However, the Adrb1-A187V mutation was shown to restore REM sleep, mitigating the sleep disturbances seen in the tauopathy model.
Implications for tau aggregation
The spread of tau protein is a critical factor in the progression of Alzheimer’s disease. Research has shown that tau can propagate transsynaptically in both human and mouse neurons. The central amygdala, a complex brain structure with diverse neuronal populations, has been identified as a key site in this process. Retrograde tracing, performed using adenoviral vectors carrying fluorescent genes, revealed that ADRB1-expressing neurons in the central amygdala form direct connections with the locus coeruleus.
To probe the impact of the Adrb1-A187V mutation on tau propagation, researchers utilized StressMarq’s Tau-441 (2N4R) P301S Mutant Pre-formed Fibrils (catalog #SPR-329). Tau fibrils were injected into the central amygdala, leading to the spread of pathogenic tau into downstream regions, including the locus coeruleus. Remarkably, the Adrb1-A187V mutation significantly reduced the spread of tau from the central amygdala to the locus coeruleus, highlighting its potential to mitigate the progression of tauopathies.
Increased wakefulness protects against tau pathology
In this study, scientists explored the relationship between tau pathology and the Adrb1-A187V mutation associated with familial natural short sleep (FNSS), a condition in which individuals require less sleep. This mutation, which promotes wakefulness, was found to mitigate neurodegenerative symptoms by restoring REM sleep and reducing the spread of tau protein. To assess tau propagation between different brain regions, the researchers employed StressMarq’s Tau-441 (2N4R) P301S Mutant Pre-formed Fibrils (catalog #SPR-329), providing critical insights into the mutation’s protective effects against tauopathies.
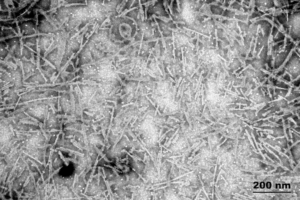
[Image from: StressMarq website] TEM imaging of StressMarq’s Tau-441 (2N4R) P301S Mutant PFFs (catalog# SPR-329).
Summary
Individuals with Alzheimer’s disease often experience sleep disturbances, including shorter sleep durations and disruptions to the sleep cycle. These disturbances can lead to anxiety, confusion, and cognitive impairment, particularly due to decreased REM sleep, which is closely associated with memory and brain function. New research conducted by Dong et al. highlights a link between tau pathology and the Adrb1-A187V mutation in the β1-adrenergic receptor (β1AR), a mutation associated with individuals who naturally require less sleep.
The Adrb1-A187V mutation was shown to protect against neurodegeneration by reducing tau aggregation in the locus coeruleus, the brain’s sleep-wake center, attenuating tau spread and restoring REM sleep. These findings shed light on molecular pathways that could be targeted to improve sleep quality, offering a potential strategy to delay the onset and progression of tauopathies such as Alzheimer’s disease.
Related StressMarq products
StressMarq’s diverse range of tau constructs enable researchers to create high-quality models for neurodegenerative diseases. This extensive portfolio includes constructs with post-translational modifications that mimic those found in human neurodegenerative disorders. These include Tau dGAE (AA 297-391) AD-mimic PFFs (catalog# SPR-502) and Tau-441 (2N4R) P301S Mutant PFFs (CHO-expressed, N-glycosylated) (catalog# SPR-516). Visit our website for more information, including the latest scientific publications using our specialized tau, alpha synuclein and amyloid beta proteins for neurodegenerative disease research.
References
- Mutant β1-adrenergic receptor improves REM sleep and ameliorates tau accumulation in a mouse model of tauopathy. Dong, Q. et al., PNAS. 2023.
Leave a Reply